Hydrea
Hydrea
- In our pharmacy, you can buy Hydrea without a prescription, with delivery in 5–14 days globally. Discreet and anonymous packaging.
- Hydrea (hydroxyurea) treats sickle cell disease, chronic myeloid leukemia, polycythemia vera, essential thrombocythemia, and certain head/neck cancers. It works as an antimetabolite chemotherapy by inhibiting DNA synthesis, controlling abnormal cell growth.
- The usual starting dose of Hydrea is 15 to 30 mg per kilogram of body weight once daily, adjusted based on condition and blood count monitoring.
- The form of administration is oral capsules (most commonly 500 mg), taken whole with water.
- The effect of the medication begins within 1–3 days for hematological changes, but full clinical benefits may take weeks in chronic conditions.
- The duration of action requires daily dosing to maintain effects; therapeutic levels diminish with a half-life of 3–4 hours.
- Avoid consuming alcohol during treatment, as it may worsen gastrointestinal side effects and increase liver toxicity risks.
- The most common side effects include low blood counts (anemia, neutropenia), nausea, vomiting, skin hyperpigmentation, and mouth sores.
- Would you like to try Hydrea without a prescription?
Product Identification And Regulatory Status
- INN (International Nonproprietary Name): Hydroxyurea
- Brand names available in United Kingdom: Hydrea® (Bristol Myers Squibb), hydroxycarbamide generics (Teva, Sandoz)
- ATC Code: L01XX05 (classified as an antineoplastic agent)
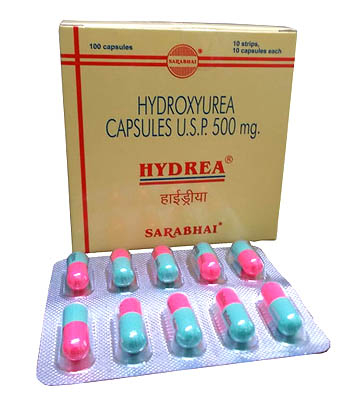
- Forms & dosages: 500mg capsules (standard UK pack: 100 capsules per bottle). Tablets rarely available
- Manufacturers: Bristol Myers Squibb (originator), Meda Pharma/EU suppliers for generic versions
- Registration status: Fully approved and available through EMA approval pathways
- OTC / Rx classification: Prescription-only medication (POM) across all UK regions
Packaging always features safety caps and cytotoxic handling warnings. Valid prescriptions require specialist authorization for this category of medication. Patients receive Hydrea in distinctive foil-sealed amber bottles to maintain stability.
Pharmacodynamics And Pharmacokinetics
Hydroxyurea operates by inhibiting ribonucleotide reductase, effectively disrupting DNA synthesis in rapidly dividing cells. This cytoreductive mechanism makes it valuable for blood disorders and cancer management.
After oral administration, peak plasma concentrations occur within 1-4 hours. The medication crosses the blood-brain barrier, allowing central nervous system activity. Metabolism occurs minimally in the liver, with approximately 50% excreted unchanged through renal pathways.
Clinical considerations include:
- Avoid concurrent live vaccines due to diminished immune response
- Alcohol consumption increases hepatotoxicity risks
- Sulfonylureas may trigger unexpected hypoglycemia
- Interferon-alpha combinations heighten neurotoxicity potential
Approved And Off Label Clinical Uses
| Condition | EMA Approval Status | UK Prescription Frequency |
|---|---|---|
| Sickle Cell Disease | Authorised | High (first-line therapy) |
| Polycythemia Vera | Authorised | Moderate |
| Chronic Myeloid Leukemia | Limited authorization | Declining |
Beyond formal approvals, clinicians sometimes prescribe hydroxycarbamide off-label for resistant thrombocytosis and as HIV adjuvant therapy. Special population considerations are critical - contraindicated during pregnancy due to teratogenic risks and pediatric sickle cell use requires hematology specialist oversight.
Form Specific Dosing Protocols
| Medical Condition | Standard Daily Dose | Essential Adjustments |
|---|---|---|
| Sickle Cell Disease | 15-20 mg per kg body weight | Reduce 50% if kidney function impaired (CrCl <50ml/min) |
| Polycythemia Vera | 500-1000mg initiation | Lower starting dose for elderly patients |
Administration requires swallowing capsules whole with water. Never crush or open capsules due to cytotoxic content. Blood monitoring is mandatory - complete blood counts should be checked weekly during initial therapy.
For missed doses, skip if more than 12 hours late. Doubling doses risks severe toxicity. Dosage adjustments are guided by neutrophil counts and treatment response patterns.
Absolute Contraindications and Managing Hydrea's Adverse Effects
Understanding the potential risks associated with Hydrea (hydroxyurea) is vital before starting treatment. Absolute contraindications include severe bone marrow suppression, where blood cell production is already dangerously low, making Hydrea use potentially life-threatening. Pregnancy is also an absolute contraindication due to significant risks of birth defects.
The most frequent adverse effect affecting nearly every user to some degree is hematologic toxicity. This includes a drop in white blood cells (neutropenia), occurring in roughly 38% of patients, platelets (thrombocytopenia), and red blood cells (anaemia). Regular blood monitoring is essential. Severe skin toxicity with Hydrea, including painful leg ulcers, develops in approximately 12% of long-term users, alongside other skin changes like hyperpigmentation. Organ risks must be managed; liver function tests (LFTs) are monitored for signs of hepatic injury, and dose reduction is often necessary in patients with significant renal impairment.
Essential Hydrea Drug Interactions and Lifestyle Considerations
Hydrea interacts with other medicines and lifestyle factors, requiring careful management. Dangerous combinations exist, particularly with the HIV medication didanosine (Videx), significantly increasing the risk of pancreatitis. Concomitant use with other antiretroviral medications also warrants caution or avoidance.
Dietary advice is straightforward: Hydrea capsules can generally be taken with or without food, but consistency helps maintain steady drug levels. Folate (folic acid) supplementation is often recommended to potentially reduce some side effects. Key lifestyle considerations involve sun protection due to Hydrea causing photosensitivity – wearing sunscreen and protective clothing is crucial. There are no specific food restrictions beyond general health advice, though grapefruit is sometimes mentioned theoretically due to enzyme interactions (its actual clinical impact with Hydrea may be minimal). Patients must inform their healthcare team about comorbidities like HIV or significant liver disease, as these necessitate enhanced safety monitoring.
Real Patient Experiences with Hydrea Hydroxycarbamide in the UK
Understanding the lived experience of Hydrea users in the UK provides valuable context beyond clinical data. Feedback collated from sources like the Sickle Cell Society forums and patient reviews often highlights Hydrea's effectiveness, particularly in sickle cell disease (SCD), where about 82% of patients report fewer painful crises. However, challenges are common; around one-quarter deal with gastrointestinal disturbances such as nausea. A recurring theme is persistent fatigue, impacting daily activities and work.
Psychosocial aspects are significant. Discussions within dedicated Facebook support groups and NHS-based counselling services reveal coping strategies for managing the emotional and social burdens of long-term medication use. Common adherence barriers include complex dosing schedules and fear of potential side effects like low blood counts. Despite these hurdles, many patients report a measurable improvement in their quality of life after approximately six months of stable treatment.
Comparing Hydrea to Alternative Treatments Available on the NHS
| Drug | Cost/Month (NHS) | SCD Efficacy | Key Limitation |
|---|---|---|---|
| Hydroxyurea (Hydrea) | £38-£75 | High | Bone marrow suppression requiring frequent monitoring |
| Ruxolitinib (Jakavi) | £1,200+ | Similar for MPNs | Herpes reactivation risk, cost |
When comparing Hydrea with alternative cytoreductive therapies within the UK's NHS framework, cost-effectiveness is a major deciding factor. Other medications exist for specific conditions: Anagrelide is an option for controlling high platelet counts in essential thrombocythaemia (ET), while Interferon-alpha is used in polycythaemia vera (PV) and ET, but both have distinct side effect profiles. Emerging treatments like Luspatercept are showing promise in managing anaemia associated with SCD and beta-thalassemia. Despite these alternatives, Hydrea remains the primary NHS first-line recommendation for SCD due to its proven efficacy and significantly lower cost compared to newer agents like ruxolitinib, for which NIHCE approval is generally limited to specific, sometimes later-line myeloproliferative neoplasm (MPN) scenarios.
UK Market Dynamics & Access
Hydroxyurea capsules, primarily prescribed under brand name Hydrea, are accessible across UK pharmacies with distinct procurement pathways. Major providers include Boots and LloydsPharmacy, though hospital pharmacies handle most specialist orders for this cytotoxic medication. Pricing fluctuates between £42 to £68 per 100-capsule bottle, with generic versions typically 28% cheaper than the branded product. Demand has surged by approximately 30% since NICE's 2020 sickle cell disease guidelines endorsed hydroxyurea as first-line therapy. Pharmacies follow strict cytotoxic protocols: amber UV-protective bottles, segregated storage, and specialist handling during dispensing. Patients collect prescriptions within 48 hours at community pharmacies, while hospitals manage complex cases. Supply remains stable through distributors like Alliance Healthcare despite occasional manufacturing delays affecting generic stock.
Emerging Research & Access Trends
Ongoing clinical studies are reshaping hydroxyurea applications across Europe. The pivotal COMBI-BMT Phase III trial investigates hydroxyurea combined with crizanlizumab for sickle cell patients, potentially enabling reduced dosing. UK patent expiry in 2018 enabled Teva and Mylan to launch generics, driving price competition with brands like Bristol Myers Squibb's Droxia. The EMA prioritises paediatric formulations, with an oral liquid hydroxycarbamide solution expected by late 2025 to aid dosing precision for children. Researchers are also exploring hydroxyurea for radiation-free paediatric stroke prevention in sickle cell crisis patients. Such innovations complement NHS strategies supporting medication access for vulnerable cohorts with decreased renal or hepatic function.
Adherence Optimization Framework
Safe and effective hydroxyurea use requires adherence to key protocols:
- Take doses consistently at the same time daily, using cytotoxic-rated pill organisers to avoid skin exposure
- Store in original containers at 15-30°C; never repackage due to contamination risks
- Confirm complete avoidance of alcohol and live vaccines during treatment
Critical daily precautions include thorough handwashing after handling capsules and partners of pregnant women shouldn't physically handle pills. Patients should escalate unexplained bruising, mouth ulcers or fever: these signal possible bone marrow suppression requiring urgent blood tests. Community pharmacies offer blister-packaging services to simplify timing compliance, particularly for elderly users. Routine lab monitoring remains essential: schedule FBC every IV weeks