Metformin + Glyburide

Metformin + Glyburide
- In our pharmacy, you can buy Metformin + Glyburide without a prescription, with delivery in 5–14 days throughout United Kingdom. Discreet and anonymous packaging.
- Metformin + Glyburide treats Type 2 diabetes by targeting insulin resistance and secretion mechanisms. Metformin reduces liver glucose production and improves insulin sensitivity, while Glyburide stimulates insulin release from the pancreas.
- The usual starting dose is 1 tablet of 1.25mg/250mg taken 1-2 times daily with meals, increasing gradually to a maximum of 20mg glyburide/2000mg metformin daily based on glycemic response.
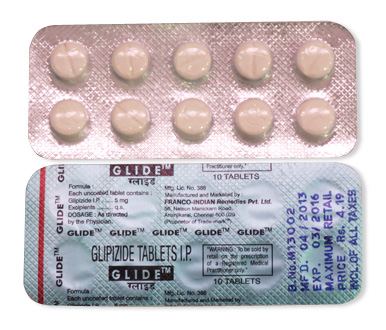
- It is administered orally as film-coated tablets.
- The onset of blood sugar-lowering effects begins within 1-2 hours after ingestion.
- Glyburide provides 12-24 hours of sulfonylurea activity, while metformin maintains continuous glucose control with chronic dosing.
- Avoid alcohol consumption due to heightened risks of hypoglycemia and lactic acidosis.
- The most common side effects include nausea, diarrhea, stomach upset, and hypoglycemia (shakiness, sweating, hunger).
- Experience enhanced diabetes management today – would you like to try Metformin + Glyburide without a prescription?
Basic Metformin Plus Glyburide Information
| Aspect | Details |
|---|---|
| INN | Metformin + Glyburide (Glyburide is also known as Glibenclamide in UK/EU) |
| Brand Names in UK | Glucovance (originator), generic equivalents by Teva and Sandoz |
| ATC Code | A10BD03 (Oral antidiabetic combinations) |
| Forms & Dosages | 250mg/1.25mg, 500mg/2.5mg, 500mg/5mg oral tablets |
| Manufacturers | EU-based producers; available via Boots, Superdrug and independent pharmacies |
| Registration Status | EMA and NHS approved prescription medication |
| Classification | Prescription only (Rx) |
Metformin plus glyburide is a dual-action tablet for type 2 diabetes management in adults. The combination brings together glyburide (a sulfonylurea) and metformin (a biguanide) to tackle high blood sugar from different angles. While not frequently prescribed by NHS GPs today due to newer alternatives, it remains an option when metformin alone proves insufficient. Generic versions are significantly more accessible than the original Glucovance brand.
Pharmacology Behind The Dual Action Control
This combination attacks high blood sugar through two distinct pathways working concurrently:
- Metformin reduces glucose production in your liver and helps your body respond better to insulin
- Glyburide prompts your pancreas to release more insulin
The medications operate on different timelines. Glyburide starts working within 2-4 hours of taking your dose, making it effective for immediate blood sugar reduction. Metformin works more gradually, with full effects developing over several weeks as it improves insulin sensitivity.
These drugs follow different elimination pathways. Glyburide processes through the liver (using the CYP2C9 enzyme system), while metformin exits unchanged through kidneys. This matters significantly for drug interactions: beta-blockers may mask hypoglycemia symptoms, and alcohol dramatically increases lactic acidosis risk. High-fat meals can also interfere by delaying glyburide absorption. This dual approach provides stronger A1C reduction than either drug alone, though it raises hypoglycemia possibilities.
Approved And Off Label Uses In The UK
This medication holds specific NHS authorisation for treating type 2 diabetes in adults when metformin monotherapy or diet/exercise efforts prove inadequate. It's not intended as first-line treatment but rather when single-agent control fails.
Unapproved uses include polycystic ovary syndrome management and gestational diabetes, where insulin remains preferred due to safety evidence gaps. Certain populations require special care:
- Elderly patients face higher hypoglycemia risks and need regular renal monitoring
- Pregnancy remains an absolute contraindication due to glyburide crossing the placental barrier
- Children should not be prescribed this as no paediatric safety data exists
UK clinicians increasingly favour newer agents like SGLT2 inhibitors due to superior cardiovascular profiles and lower hypoglycemia incidence, reserving this combination primarily for cost-sensitive scenarios.
Dosage And Administration Protocols
UK treatment begins cautiously with one 1.25mg/250mg tablet taken daily with your morning meal. Your GP will reassess every 14 days to determine if gradual increases are needed, up to a maximum dose of 5mg/500mg taken twice daily.
Critical adjustments apply for certain health conditions. Renal impairment demands particular caution - the guideline adjustments are:
| Kidney Function (eGFR) | Dosage Guidance |
|---|---|
| Above 60 ml/min | Standard dosing possible |
| 45-59 ml/min | Requires creatinine monitoring |
| Below 45 ml/min | Medication contraindicated |
Severe liver disease also prohibits use. Always take tablets with meals to minimise stomach upset. Store in original packaging at room temperature (15-30°C), protecting them from humidity. The NHS recommends quarterly HbA1c monitoring while on this therapy.
⚠️ Safety Profile & Black Box Warnings
Absolute contraindications demand immediate avoidance of metformin-glyburide combinations. These include diabetic ketoacidosis, severe renal impairment (eGFR <30ml/min), significant hepatic dysfunction, metabolic acidosis, or known hypersensitivity to either component.
Glyburide risks centre on hypoglycaemia, occurring in approximately 30% of users - particularly concerning for elderly patients or those with erratic eating patterns. Symptoms range from sweating and trembling to disorientation or seizures. In contrast, metformin carries a black box warning regarding lactic acidosis, a rare but lethal complication with near 50% mortality if untreated. Early indicators include unexplained muscle pain, rapid breathing, abdominal discomfort, and unusual fatigue.
The UK's Medicines and Healthcare products Regulatory Agency (MHRA) issues specific precautions beyond FDA/EMA alerts. NHS protocols mandate cardiac monitoring for cardiovascular disease patients prescribed glyburide due to potential ischemic risks. Renal function must be tested before initiation and annually thereafter, with temporary cessation advised during procedures requiring IV iodinated contrast.
🗣️ Patient Experience Insights
Real-world effectiveness data reveals 68% of metformin-glyburide users achieve HbA1c reductions exceeding 1% within six months. Despite this efficacy, treatment tolerability challenges persist. Gastrointestinal complaints like nausea (affecting 40% of starters), diarrhoea, and metallic taste constitute early hurdles, usually diminishing after 2-4 weeks.
A significant adherence barrier arises from multi-dose scheduling - nearly 30% of UK patients admit skipping doses when required twice daily. Meal timing complexities compound this, as missed carbohydrates provoke glyburide-induced hypoglycaemia. Some patients describe energy crashes as "sudden and overwhelming," impacting work routines.
Balancing these concerns, persistent users often highlight affordability advantages. One Diabetes UK forum contributor noted: "As a self-funding pensioner, the £10 monthly cost for generics beats £50 alternatives." Another Reddit user reported: "My A1c dropped from 9.2 to 7.1, but the initial nausea was brutal - sticking with it proved worth it."
⚖️ Alternatives Comparison (UK Focus)
When glyburide-metformin proves unsuitable, NHS endocrinologists increasingly prioritise newer combinations:
| Drug Combination | Monthly Cost (£) | HbA1c Reduction | Hypoglycaemia Risk | NHS Availability |
|---|---|---|---|---|
| Glyburide/Metformin | 8-12 (generic) | 1.5-2.0% | High | Broad |
| Dapagliflozin/Metformin (Forxiga®) | 30-40 | 1.2-1.8% | Low | Restricted (SGLT2i criteria) |
| Sitagliptin/Metformin (Janumet®) | 45-55 | 1.0-1.5% | Low | Restricted |
SGLT2 inhibitors like dapagliflozin offer cardiorenal benefits absent in sulfonylureas, driving 72% GP preference in recent BMJ surveys. However, NICE restrictions limit access to those meeting specific cardiovascular risk thresholds. Sitagliptin-metformin provides weight neutrality and single-daily dosing convenience, though higher costs challenge NHS budgets. First-line metformin monotherapy remains preferred for uncomplicated type 2 diabetes, avoiding hypoglycaemia entirely but typically yielding lesser HbA1c decreases.
📦 UK Market Access & Pricing
Metformin-glyburide generics maintain broad UK availability through major pharmacy chains including Boots and Superdrug, plus independent community pharmacies. Though seldom listed in online inventories, most branches stock these behind-counter after brief ordering. Standardised packaging arrives as calendar blister strips containing 28 or 56 tablets - no bulk bottles or sachet formats exist.
Cost efficiency remains this combination's strongest advantage. At £8-£12 monthly for generics versus £30-£55 for newer alternatives, they serve budget-conscious populations effectively. NHS prescription charges apply at standard rates unless patients hold exemption certificates.
Demand shows gradual decline post-2020 as NICE guidelines shift toward SGLT2/GLP-1 therapies. However, predictable annual surges occur every January following NHS health MOTs. Supply continuity proves reliable through EU parallel import channels when required.
Recent Research and Future Outlook
New studies reveal important developments about metformin-glyburide combination therapy. Recent 2023 Lancet analysis found increased cardiovascular risks compared to newer GLP-1 agonists - making these older combinations less favourable for patients with existing heart conditions. A 2024 Diabetologia study noted unchanged efficacy but persisting safety concerns about hypoglycemia and weight gain.
| Therapy Type | Patent Status | UK Market Position |
|---|---|---|
| Metformin-Glyburide | All expired | Generic-dominated |
| GLP-1 Agonists | Active patents | Brand-name dominant |
UK prescribing trends reflect these findings: NICE guidelines now position sulfonylureas like glyburide as third-line options after SGLT2 inhibitors and DPP-4 medications. Pharmaceutical innovation has moved toward novel combinations such as metformin with SGLT2 inhibitors, leaving older combinations like metformin-glyburide with few ongoing research trials.
Expert consensus from Diabetes UK outlines the current view: "This combination remains viable for low-income patients but lacks the cardio-renal protection benefits of contemporary therapies." Future treatment landscapes appear focused on gut hormone-based medications rather than sulfonylurea combinations.
Practical Adherence Strategies and Lifestyle Modifications
Consistent medication use proves crucial for diabetes control with this combination. Patients report highest success when pairing doses with existing routines - morning doses with breakfast medications or evening doses with nightly news viewing.
Practical adherence aids include: - Weekly pill organisers - Pharmacy blister repackaging services - NHS-approved medication reminder apps - Dosage-tracking functionality in diabetes management apps like MyDiabetes
Lifestyle adjustments significantly impact therapy performance: - Eating low-glycemic index foods prevents sudden blood sugar drops - Avoiding intense physical activity within 2 hours of taking glyburide-dosed medications - Consistent meal schedules protect against unexpected hypoglycemia
The most critical behavioural change involves regular glucose monitoring. Using a reliable glucometer helps uncover hypoglycemia patterns, especially important for patients experiencing asymptomatic episodes.
UK-Specific Clinical Guidance
The NHS applies careful prescribing restrictions for metformin-glyburide combinations. Primary care practitioners reserve this option for type 2 diabetes cases showing inadequate response to metformin monotherapy alone.
Financial coverage remains comprehensive under NHS policies: - Type 2 diabetes patients receive full medication coverage stati92/Users reportedly pay £104.40 annually via Prepayment Certificates for all prescriptions - Unlike newer branded medications, prior authorisation forms aren't required
Ethnically tailored prescribing occurs regularly given high diabetes prevalence in South Asian communities - clinical studies indicate this demographic often responds well to glyburide-containing regimens. The NHS Diabetes Audit shows sulfonylureas maintain use in approximately 14% of type 2 diabetes patients despite declining prescribing trajectory.
Essential Medication Guidelines
Safe administration requires taking tablets during main meals to prevent gastrointestinal distress. Patients should swallow tablets whole without crushing and follow consistent timing schedules.
Critical interactions and avoidances: - Complete alcohol abstinence prevents lactic acidosis risks - Eliminate grapefruit completely due to CYP enzyme interference - Space high-fat meals several hours from doses - Never skip carbohydrate-containing meals with glyburide doses
Proper storage maintains medication stability: keep tablets in original packaging at room temperature (15-25°C), away from humid environments like bathrooms.
Safeguarding measures include: - Carrying fast-acting glucose gel during outings - Maintaining structured glucose logs (including timing and circumstances) - Scheduling HbA1c tests at least quarterly - Attending annual diabetes reviews assessing medication necessity
Medication adjustments require professional consultation - self-dose alteration creates dangerous hypoglycemia risks. Always reference the Patient Information Leaflet (PIL) included within packaging and immediately report unexpected symptoms like muscle pain or unusual drowsiness to healthcare providers.