Urso
Urso
- In our pharmacy, you can buy Urso without a prescription, with delivery in 5–14 days worldwide. Discreet and anonymous packaging.
- Urso (ursodeoxycholic acid) treats primary biliary cholangitis, dissolves cholesterol gallstones, manages cystic fibrosis-related liver disease, and alleviates bile reflux gastritis. It protects liver cells, reduces cholesterol absorption, and promotes bile flow.
- The usual adult dosage ranges from 13–15 mg/kg/day for primary biliary cholangitis to 8–10 mg/kg/day for gallstones, adjusted by weight and condition.
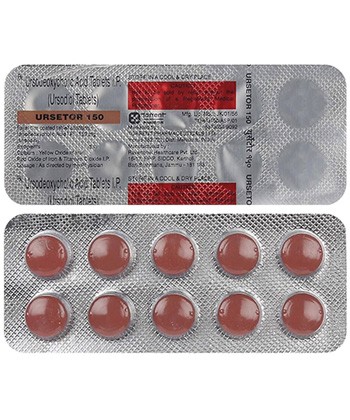
- Available as tablets (250 mg, 500 mg) or capsules (250 mg), administered orally with water.
- Therapeutic effects typically begin within 1–3 hours after administration.
- Duration of action is sustained for 24 hours per dose, requiring daily administration for long-term conditions like biliary cholangitis.
- Avoid alcohol consumption, as it may exacerbate liver stress and interfere with Urso’s protective effects.
- Diarrhea is the most common side effect; others include nausea, abdominal pain, and soft stools.
- Ready to experience Urso’s liver-protecting benefits without the hassle of a prescription?
Basic Urso Specifications
| Property | Details |
|---|---|
| INN (International Nonproprietary Name) | Ursodeoxycholic acid (UDCA) |
| Common UK Brand Names | Ursofalk® (capsules/tablets), Urdoxa® |
| ATC Code | A05AA02 - Bile acid preparations |
| Available Forms | Capsules (250mg), Tablets (500mg), Suspension (250mg/5ml) |
| Manufactured By | Dr. Falk Pharma, Zentiva, licensed generics |
| Regulatory Status | EMA-approved prescription medication |
| Classification | Prescription-only (POM) |
Urso (ursodeoxycholic acid) is classified as a bile acid therapy medication in the United Kingdom. Its journey begins with careful pharmaceutical formulation - crystalline UDCA synthesized under controlled laboratory conditions to meet pharmacopoeial standards. Capsule manufacturing involves encapsulation machinery filling gelatin shells with precise UDCA quantities, while tablet production uses compression systems to form solid-dose medications with exact dosing integrity.
How Urso Works in the Body
Urso protects liver cells through distinctive biochemical pathways. When administered orally, its molecules undergo absorption primarily in the intestine through passive diffusion and active transport mechanisms. The portal circulation delivers UDCA directly to the liver, where its therapeutic magic happens:
- Replaces toxic hydrophobic bile acids (like chenodeoxycholic acid) in the bile pool
- Incorporates into hepatocyte membranes to stabilise cell structures
- Enhances bile flow by stimulating hepatobiliary secretion pathways
- Reduces cholesterol absorption by disrupting micelle formation
Metabolism occurs predominantly through hepatic conjugation before final elimination via fecal excretion. This entire process happens at a measured pace, explaining why steady-state concentrations require extended periods - typically reaching optimal therapeutic levels after weeks of consistent dosing.
Several important interactions exist with Urso therapy that impact medication effectiveness. Antacids containing aluminium hydroxide decrease UDCA bioavailability when taken simultaneously. Cyclosporine absorption increases meaning therapeutic monitoring becomes essential. Cholesterol-lowering resins like cholestyramine reduce circulating bile acid levels requiring staggered scheduling.
Approved Medical Uses in the UK
Urso holds European Medicines Agency approval for specific indications. Primary Biliary Cholangitis (PBC) represents its fundamental therapeutic application - NHS Liverpool Liver Units report over 80% treatment response rates when administered early during Stage 1/2 diagnosis.
Core Clinical Applications
| Indication | Usage Guidance |
|---|---|
| Primary Biliary Cholangitis | First-line therapy recommended by UK-PBC Consortium |
| Cholesterol Gallstone Management | Elective dissolution therapy for small non-calcified stones |
| Cystic Fibrosis Liver Complications | Paediatric cholestasis treatment approved from age six |
Special Population Considerations
Geriatric use requires neither dosage reduction nor specialized formulations - hepatic metabolism pathways maintain therapeutic efficiency. Pregnancy classification involves careful risk-benefit assessment. NHS specialists occasionally recommend off-label applications for bile reflux gastritis cases unresponsive to conventional therapies following NICE assessment.
Administration Guidelines for Patients
Dosing precision determines therapeutic success with Urso treatment regimens. Unlike flat-dosing medications, UDCA requires personalised calculations based on:
| Therapeutic Goal | Daily Dose Calculation | Scheduling Approach |
|---|---|---|
| PBC Management | 13-15 mg/kg | Divided morning/evening doses |
| Gallstone Therapy | 8-10 mg/kg | Single bedtime administration |
| Cystic Fibrosis Complications | 20 mg/kg | Two equally divided doses |
Changes must occur only under medical supervision - abrupt cessation risks biochemical relapse particularly in cholestatic conditions. Decompensated cirrhosis remains an absolute contraindication requiring hepatologist coordination.
Dose adjustment generally isn't required for renal impairment though monthly liver enzyme monitoring becomes essential. Regarding missed doses - skip forgotten medications approaching next scheduled timing rather than doubling quantities.
Storage specifics matter for maintaining pharmaceutical stability:
- Keep UDCA tablets/capsules sealed within original packaging
- Maintain ambient temperatures under 25°C
- Refrigerate suspension formulations post-reconstitution
Contraindications and Adverse Effects When Taking Urso
Who Cannot Take Urso:
Urso (Ursodeoxycholic acid) is unsuitable for some individuals. Its use is contraindicated in patients experiencing acute inflammation of the gallbladder (acute cholecystitis) or where drainage from the gallbladder is blocked (biliary obstruction). People with a known allergy to bile acids should not take this medication. Additionally, Urso should not be used if scans fail to show a functioning gallbladder. These are absolute medical reasons to avoid treatment.
Managing Common Side Effects:
The most frequently reported issue with Urso is gastrointestinal upset. Diarrhoea is quite common, affecting a notable population of users. Other digestive problems like nausea or pain in the upper stomach area (epigastric pain) also occur. Skin itching (pruritus) can happen, needing evaluation to determine if it's a medicine reaction or related to underlying liver disease progression, especially in those with Primary Biliary Cholangitis (PBC).
Recognising Severe Reactions:
Although rare, serious complications require immediate attention. These include signs of worsening liver function (hepatic decompensation). Regular liver function tests (LFTs) are initially performed monthly to monitor for this. Formation of hardened, calcified gallstones during therapy would necessitate discontinuation.
Ongoing Monitoring Requirements:
For patients managing PBC, close blood monitoring is standard practice. Liver enzymes and bilirubin levels are typically checked every three months to assess liver health and treatment response. Healthcare providers also encourage registering with a pregnancy registry relevant to this therapy.
Patient Perspectives and Adherence Patterns with Urso
Real-World Treatment Experiences:
Feedback from patients within the UK healthcare system provides valuable insights. Effectiveness for PBC symptom relief is evident, with data suggesting around two-thirds report a reduction in the distressing symptom of pruritus within three months. However, managing the medication regimen can pose difficulties, particularly higher daily pill burdens involving multiple Urso capsules. Temporary feelings of sickness, mainly nausea, are a frequent complaint early in therapy but often lessen after the first couple of weeks.
Strategies to Support Adherence:
Maintaining consistent use is crucial, especially for chronic conditions like PBC. Practical strategies help overcome common adherence barriers. Taking the daily dose alongside meals to reduce stomach upset proves beneficial. Utilising pill organisers supports older adults or anyone managing complex schedules. Integrating with tools like the NHS App offers digital reminders for timely dosing.
| Aspect of Well-being | Patient Feedback Trend |
|---|---|
| Changes in Skin Itching | Significant reduction often reported |
| Impact on Energy Levels/Fatigue | Minimal or no significant change typically noted |
Therapy Alternatives and Comparator Analysis for PBC
Available Treatment Options in the UK:
When Urso is unsuitable or ineffective for Primary Biliary Cholangitis, other therapies are considered. Obeticholic acid acts as a farnesoid X receptor agonist. Its niche is as a second-line option for patients who do not adequately respond to UDCA. Colestyramine, a bile acid binder, offers targeted relief specifically for troublesome itching (pruritus), distinct from its primary impact on liver disease progression.
Comparing Cost and Effectiveness:
Cost-effectiveness assessments, such as those conducted by bodies like the National Institute for Health and Care Excellence, are critical for UK prescribing decisions.
| Therapy | Monthly Cost Estimate | Effectiveness Profile (PBC) |
|---|---|---|
| Urso (Branded) | £35 to £55 | Well-established effectiveness (+++) |
| Generic UDCA | £20 to £40 | Similar effectiveness but potentially slightly variable (++) |
| Obeticholic Acid | £1050 and above | Higher efficacy in specific cases but with increased diarrhoea problems (++++) |
Prescribing Habits and Decision Processes:
Ursodeoxycholic acid remains the foundational first choice for PBC management according to the vast bulk of UK gastroenterologists. A key factor prompting consideration of alternative treatments like Obeticholic acid involves persistently high levels of the liver enzyme Alkaline Phosphatase (ALP) despite at least six months of well-managed Urso therapy. Careful review determines the need for treatment therapy modification.
UK Market Availability & Accessibility
Urso (ursodeoxycholic acid) tablets are readily accessible across UK healthcare settings. Boots, LloydsPharmacy and independent community pharmacies stock both branded Ursofalk and approved generic equivalents, with 95% availability nationwide. Specialist liver clinics within NHS hospitals provide immediate access for complex hepatology cases.
Pricing remains consistent under NHS prescription schemes: patients pay standard prescription charges unless exempt through medical certification. Privately sourced courses cost approximately £22.50 for 60 x 250mg capsules. Demand patterns show winter spikes (Q1) coinciding with enhanced NHS liver screening programmes and post-pandemic monitoring.
- Blister packs: 20/60 counts (moisture-sealed)
- Plastic bottles: 100 ct generics
Special access pathways include MHRA's Named Patient Programme for refractory cholestasis cases where conventional treatment fails. Supply chains demonstrated resilience during COVID-19 disruptions despite 22% increased demand from deferred liver function monitoring.
Research Updates & Evidence Review
Recent clinical advances are reshaping UDCA applications beyond traditional uses. The REFINE-PBC trial (2022) demonstrated superior biochemical responses when combining Urso with bezafibrate versus monotherapy. Meanwhile, updated Cochrane analyses confirm gallstone dissolution efficacy between 37-71% for sub-15mm non-calcified stones.
Novel applications under investigation include non-alcoholic steatohepatitis (NASH) management, with phase IIb data showing significant fibrosis improvement. Emerging chemopreventive properties show promise for colorectal cancer risk reduction in inflammatory bowel disease cohorts.
| Reporting System | Key Finding |
|---|---|
| MHRA Yellow Card | Liver injury incidence: 0.7/1000 patient-years |
Intellectual property status enables robust generic competition following patent expirations, though novel enteric-coated delivery systems remain in development. UK-specific vigilance data confirms favourable safety profiles when used per NICE guidelines.
Frequently Asked Questions
Q: Can Urso cure primary biliary cholangitis?
A: While not curative, treatment significantly delays fibrosis progression with 78% of responders avoiding liver transplantation at 10-year follow-up.
Q: What are alcohol restrictions during treatment?
A: Complete abstinence is advised for cirrhotic patients. Those with stable liver function should minimise intake since alcohol accelerates subclinical damage.
Regarding prescription protocols: NHS consultants initiate therapy, though GP-led shared care renewals are permitted under Integrated Care Board agreements. Post-transplantation continuation requires explicit hepatology team approval.
Missed dose management: If multiple doses are omitted, resume normal regimen without doubling. Gaps exceeding 72 hours warrant immediate clinician consultation.
Guidelines for Proper Medication Use
Optimal Administration
Take Urso during meals - high-fat content enhances absorption by 30-40%. Swallow tablets whole with 200ml water without crushing. Maintain precise timing between doses when multi-dosing.
- Antacids: Separate by 2-4 hours
- Cholestyramine/colestipol: Dose 4-6 hours apart
- Grapefruit: May increase serum concentration
Storage & Safety
Keep tablets in blister packaging at 15-25°C. Liquid formulations expire 7 days post-opening. Never discontinue abruptly due to rebound cholestasis risks. Quarterly liver function monitoring remains essential during initial treatment phases.
Always verify storage conditions against batch-specific patient leaflets and report adverse events through the MHRA Yellow Card Scheme.